Overview
Garfinkel's ethnomethodology plays a crucial role in enhancing immigrant healthcare by highlighting the significance of understanding the social interactions and cultural contexts that shape patient experiences. This approach fosters positive relationships and improves communication through cultural competency and reflexivity. As a result, healthcare providers can build trust, increase satisfaction, and ultimately improve health outcomes for immigrant populations.
We understand the challenges faced by these communities, and by embracing these principles, we can ensure that every patient feels valued and supported in their healthcare journey.
Introduction
Garfinkel's ethnomethodology reveals the complex social dynamics shaping healthcare interactions, particularly for immigrant populations navigating challenging medical systems. This approach deepens our understanding of patient-provider relationships and underscores the vital role of cultural competency in delivering effective care. Yet, many immigrants encounter significant barriers—language obstacles and systemic biases—that can obstruct their access to essential healthcare.
How can healthcare providers harness ethnomethodology to foster a more inclusive environment, addressing these challenges and improving health outcomes for diverse communities? We’re in this fight together.
Garfinkel's Ethnomethodology: Understanding Social Interactions in Healthcare
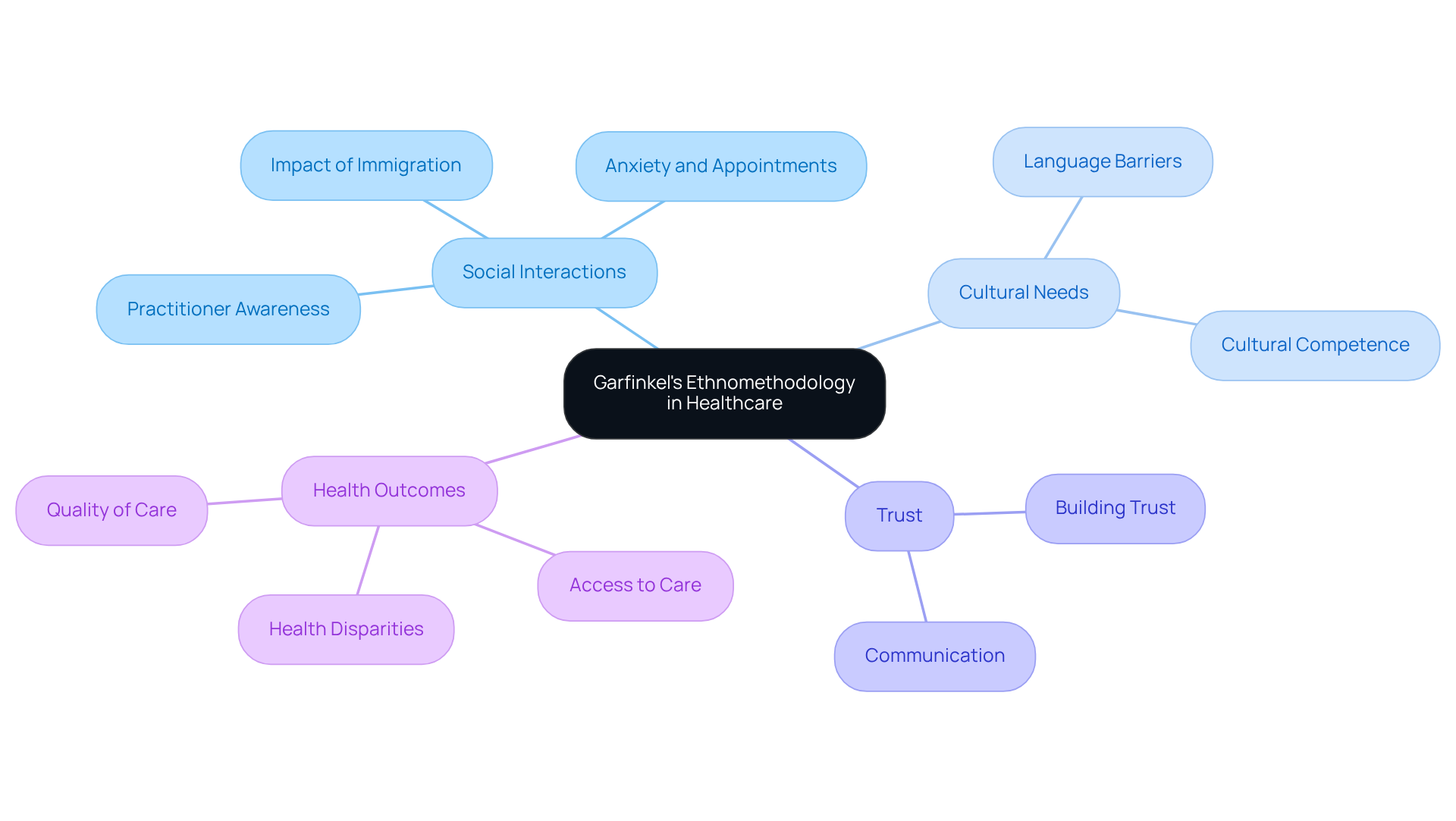
Garfinkel's ethnomethodology uncovers the everyday practices that individuals utilize to navigate their social environments. In the realm of medical services, this perspective is vital for understanding the relationships between those seeking care and practitioners, including Garfinkel. Such dynamics can significantly influence the quality of assistance provided.
For foreign-born medical professionals, grasping these interactions is essential to foster an environment where individuals feel valued and understood. Studies indicate that positive social interactions lead to increased trust, improved communication, and ultimately better health outcomes for individuals from abroad. Yet, many newcomers experience anxiety regarding immigration enforcement, causing them to miss medical appointments and .
When medical practitioners are attuned to the cultural and linguistic needs of their patients, it not only elevates the quality of care but also alleviates the isolation and anxiety that many newcomers face in clinical settings. As Dr. Woolhandler points out, "Patients are canceling health care appointments, skipping appointments without canceling, and failing to respond to outreach more often," underscoring the urgent need for supportive social interactions.
By prioritizing these connections, medical systems can significantly enhance the overall health experience for foreign populations, ensuring they receive the respect and attention necessary for optimal health management. Moreover, understanding the broader implications of immigration policies on medical access is crucial for addressing the challenges faced by individuals from abroad.
Reflexivity in Ethnomethodology: Enhancing Patient-Caregiver Relationships
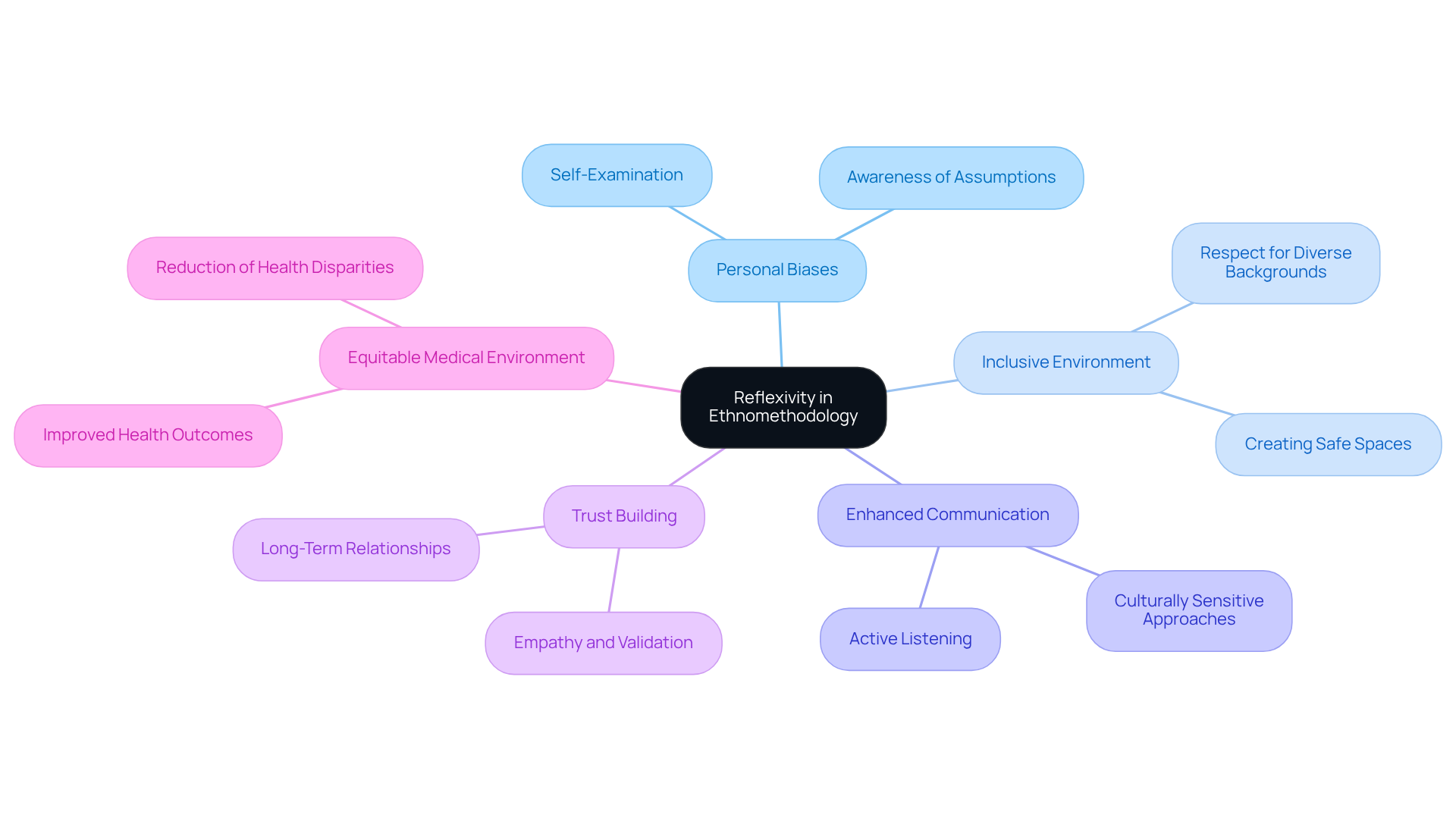
Reflexivity is a vital practice for medical professionals. It requires a thoughtful examination of personal biases and assumptions during client interactions. This self-awareness is particularly important when working with newcomers, who often feel marginalized within the medical system.
By actively engaging in reflexive practices, caregivers can create an inclusive environment that respects diverse backgrounds and experiences. This approach not only enhances communication but also builds trust, allowing immigrant individuals to feel more comfortable and valued in their medical journeys.
Experts highlight that acknowledging and addressing biases can significantly improve relationships with clients, leading to better health outcomes. Ultimately, the impact of reflexivity extends beyond individual interactions, contributing to a more for everyone.
Breaching Experiments: Revealing Norms in Healthcare Interactions
Breaching experiments reveal how immigrant individuals confront cultural differences and systemic barriers in medical systems. These insights are crucial, especially as nearly one-third of Latinx individuals report limited English proficiency, complicating their interactions with healthcare providers. This language barrier often leads to misunderstandings and dissatisfaction with care, leaving individuals feeling unheard and unsupported.
Cultural norms play a significant role in these interactions. Many Latinx individuals prioritize family involvement in healthcare decisions, reflecting the cultural value of familismo. This approach can clash with the more individualistic perspective common in U.S. healthcare, resulting in confusion and frustration during consultations. Individuals may hesitate to voice their needs or preferences, feeling caught between two worlds.
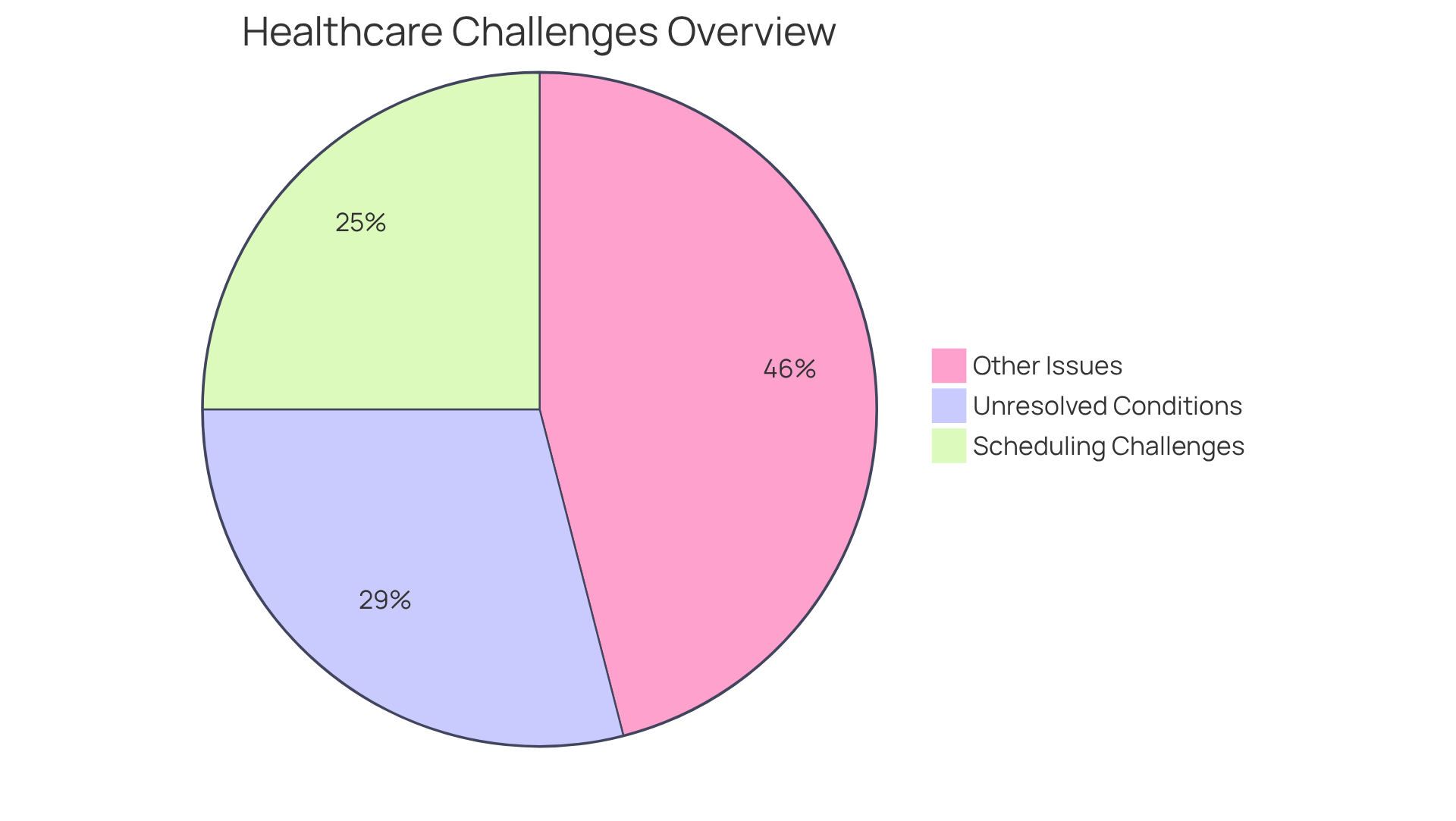
Statistics show that:
- 25% of immigrant adults face challenges in scheduling appointments, often worsened by language barriers and cultural misunderstandings.
- 29% of Spanish-speaking individuals report unresolved medical conditions after a doctor’s visit, underscoring the consequences of communication barriers.
By conducting breaching experiments, medical providers can uncover these hidden expectations and adapt their practices. This understanding is essential for fostering an inclusive atmosphere that respects and supports the diverse cultural backgrounds of newcomers, ultimately enhancing their medical experiences. We’re here to fight for your family and in the healthcare system.
Rationality in Ethnomethodology: Making Informed Healthcare Decisions
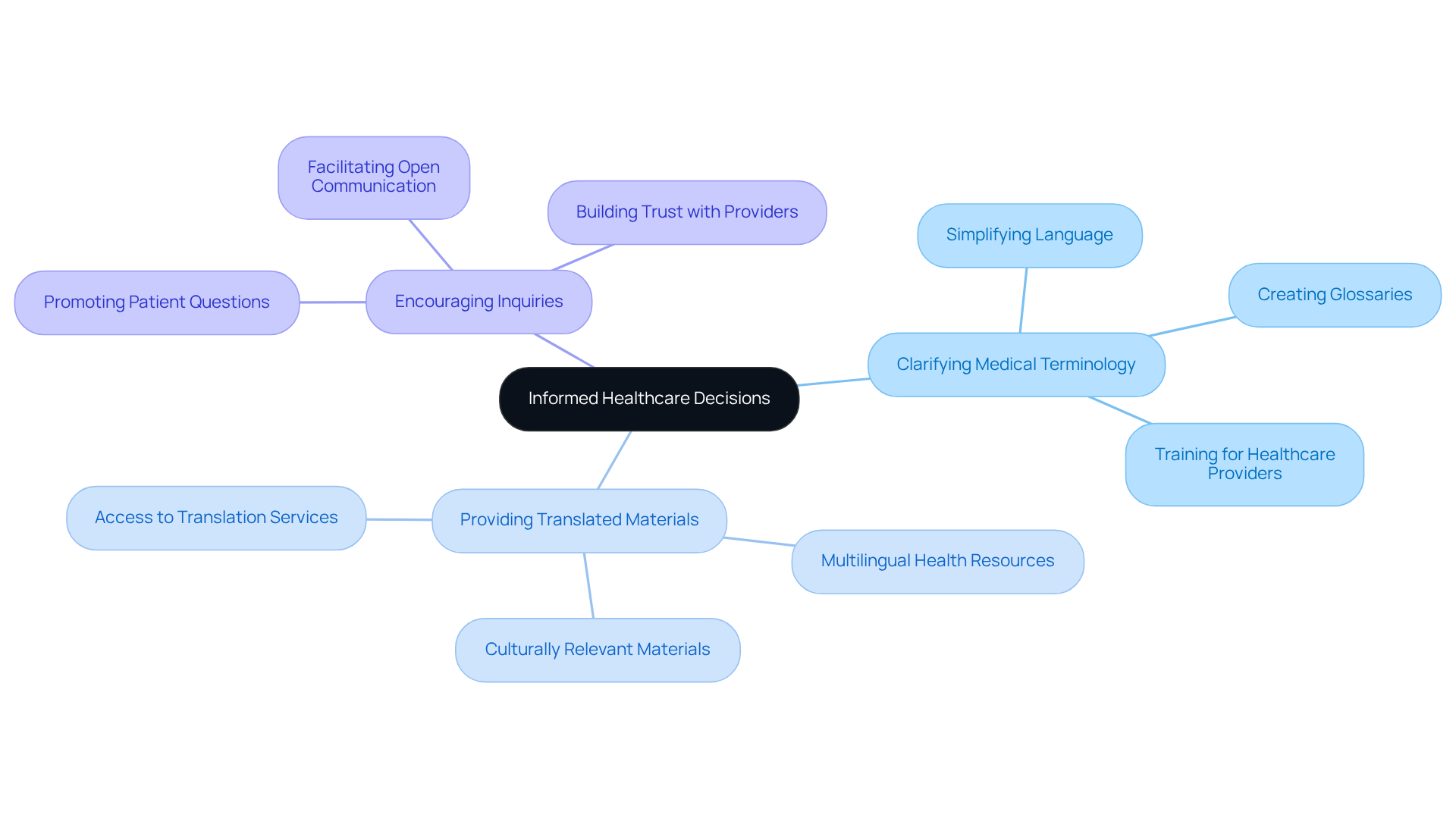
Rationality in ethnomethodology highlights the critical need for informed decision-making in medical care. For immigrant individuals, having access to clear and relevant information about health options is essential. This can be achieved by:
- Clarifying medical terminology, making the information more understandable and enabling individuals to actively participate in their medical choices.
- Providing translated materials, which is vital; it bridges language gaps and ensures that individuals fully comprehend their medical conditions and treatment options.
- Encouraging inquiries, which nurtures a collaborative decision-making process, allowing medical practitioners to address specific concerns and enhance understanding.
Research shows that significantly improves outcomes for individuals, especially within diverse populations. By prioritizing clarity and understanding, medical professionals can create a more inclusive environment that supports the health and well-being of migrant communities.
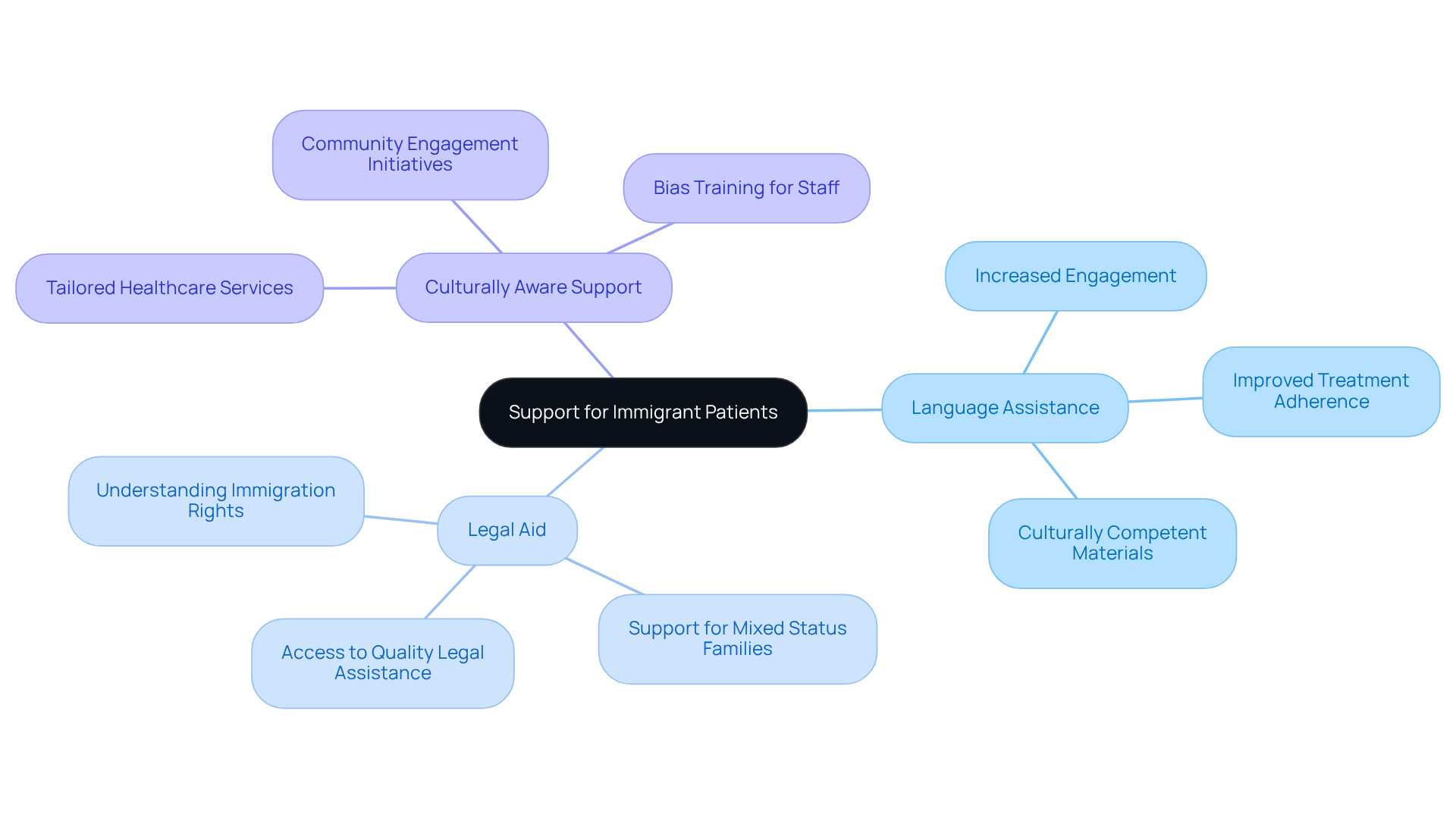
Service Lines in Healthcare: Structuring Support for Immigrant Patients
Establishing distinct service pathways in the medical field is vital for enhancing the experience of individuals, especially newcomers navigating unfamiliar systems. Have you ever felt lost in accessing healthcare? Creating specialized routes for services like language assistance, legal aid, and culturally aware support can significantly improve the help offered to immigrant individuals. For instance, healthcare organizations investing in robust language services have seen increased engagement and adherence to treatment plans. Effective communication is crucial—language barriers can lead to misunderstandings and reduced access to necessary care.
The Vasquez Law Firm exemplifies this commitment by providing specialized services in and assertive criminal defense representation. They ensure clients have access to quality legal assistance without upfront costs. Their focus on the Hispanic community, along with adaptable payment options and direct attorney access, further enhances the support available to these individuals. We understand how overwhelming this feels. By prioritizing organized support frameworks, service providers can create an inclusive atmosphere that meets the specific needs of foreign populations, ultimately promoting improved health outcomes. Your future matters to us—let's navigate this journey together.
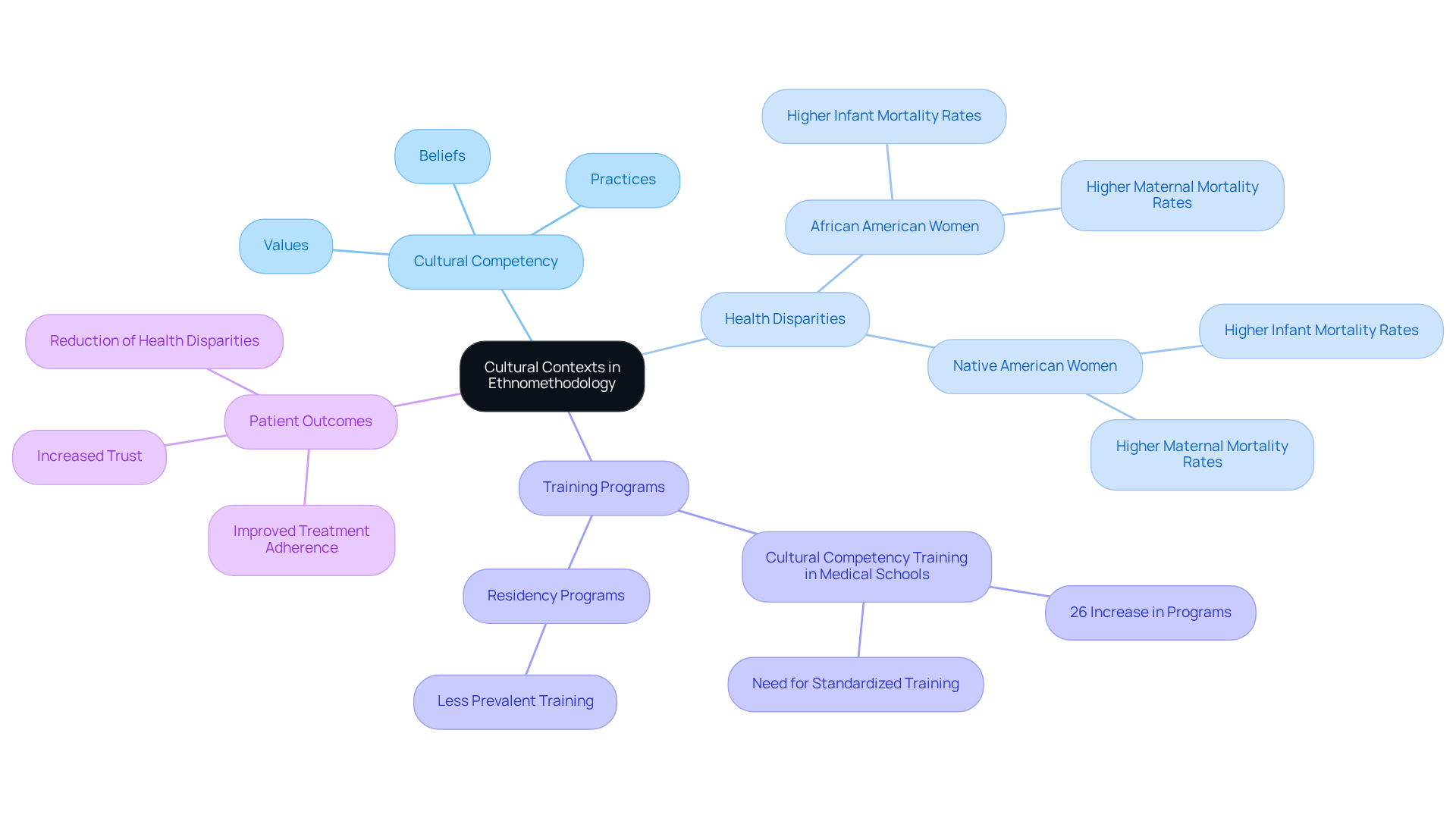
Cultural Contexts in Ethnomethodology: Tailoring Care for Diverse Populations
Understanding the is crucial for delivering effective healthcare. Cultural beliefs, practices, and values shape health behaviors, influencing how individuals perceive and respond to medical care. A 2016 study highlighted a 26% increase in programs mandating cultural competency training in medical schools, underscoring its growing importance.
Healthcare providers must prioritize cultural competency training to tailor their approaches, ensuring treatment plans respect and incorporate each individual's unique cultural background. This not only builds trust but also enhances involvement and compliance with treatment, ultimately leading to better health outcomes.
As Edward Pingenot, DO, states, "Cultural competency training in medical schools and residency programs is a crucial step toward establishing a more equitable and inclusive system of care." By recognizing and addressing the diverse cultural needs of their patients, medical professionals can create a more inclusive and effective healthcare environment.
Additionally, addressing health disparities, such as the higher rates of infant and maternal mortality among African American and Native American women, emphasizes the necessity of cultural competency in improving overall health outcomes.
The case study on the "Impact of Cultural Competency on Health Outcomes" demonstrates that true cultural competence is measurable and has been shown to enhance health results, reduce disparities, and improve patient-centered support.
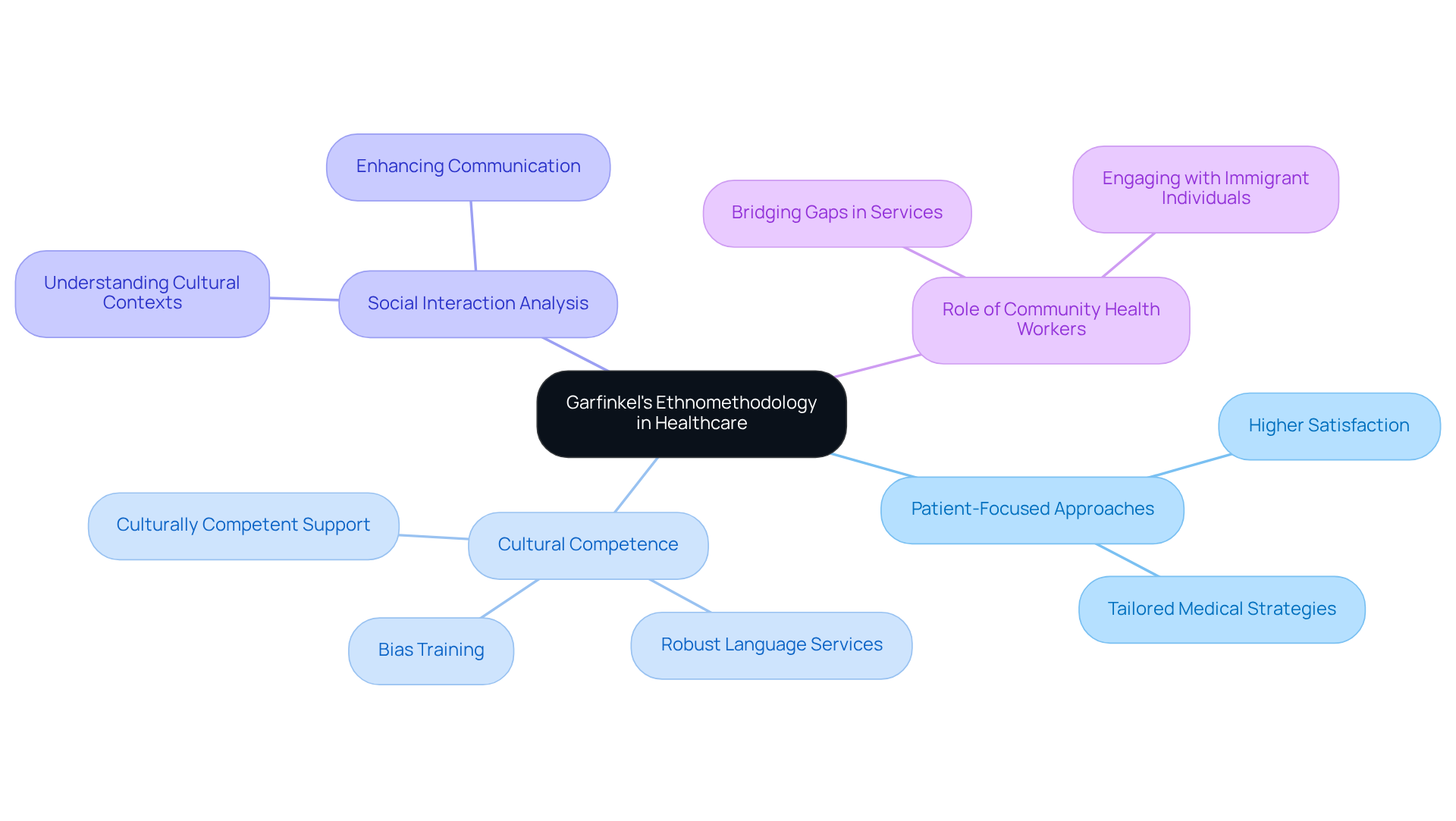
Influence of Garfinkel's Ethnomethodology on Modern Healthcare Practices
Garfinkel's ethnomethodology has significantly influenced modern medical practices by emphasizing the need for patient-focused approaches and the examination of social interactions. This method allows medical professionals to better understand the , who often encounter distinct challenges in accessing treatment. Research shows that adopting person-focused care models can lead to higher satisfaction among these groups, highlighting the effectiveness of tailored medical strategies.
Moreover, experts agree that understanding the cultural contexts and social dynamics of newcomers is vital for improving health outcomes. By fostering an environment where individuals feel recognized and valued, medical professionals can enhance communication and adherence to treatment plans. Recent reports indicate that healthcare facilities are increasingly embracing these principles, recognizing the importance of robust language services and culturally competent support to empower foreign-born individuals.
Incorporating social interaction analysis into medical practices not only elevates the quality of care but also addresses the emotional and psychological needs of immigrant individuals. This holistic approach is essential in navigating the complexities of medical access, ultimately leading to better health outcomes and a more equitable healthcare system. Additionally, requiring staff to participate in bias training can further enhance the cultural competence of service providers, ensuring they are equipped to meet the diverse needs of those they serve. Community health workers also play a crucial role in engaging with immigrant individuals, helping to bridge gaps in services and support.
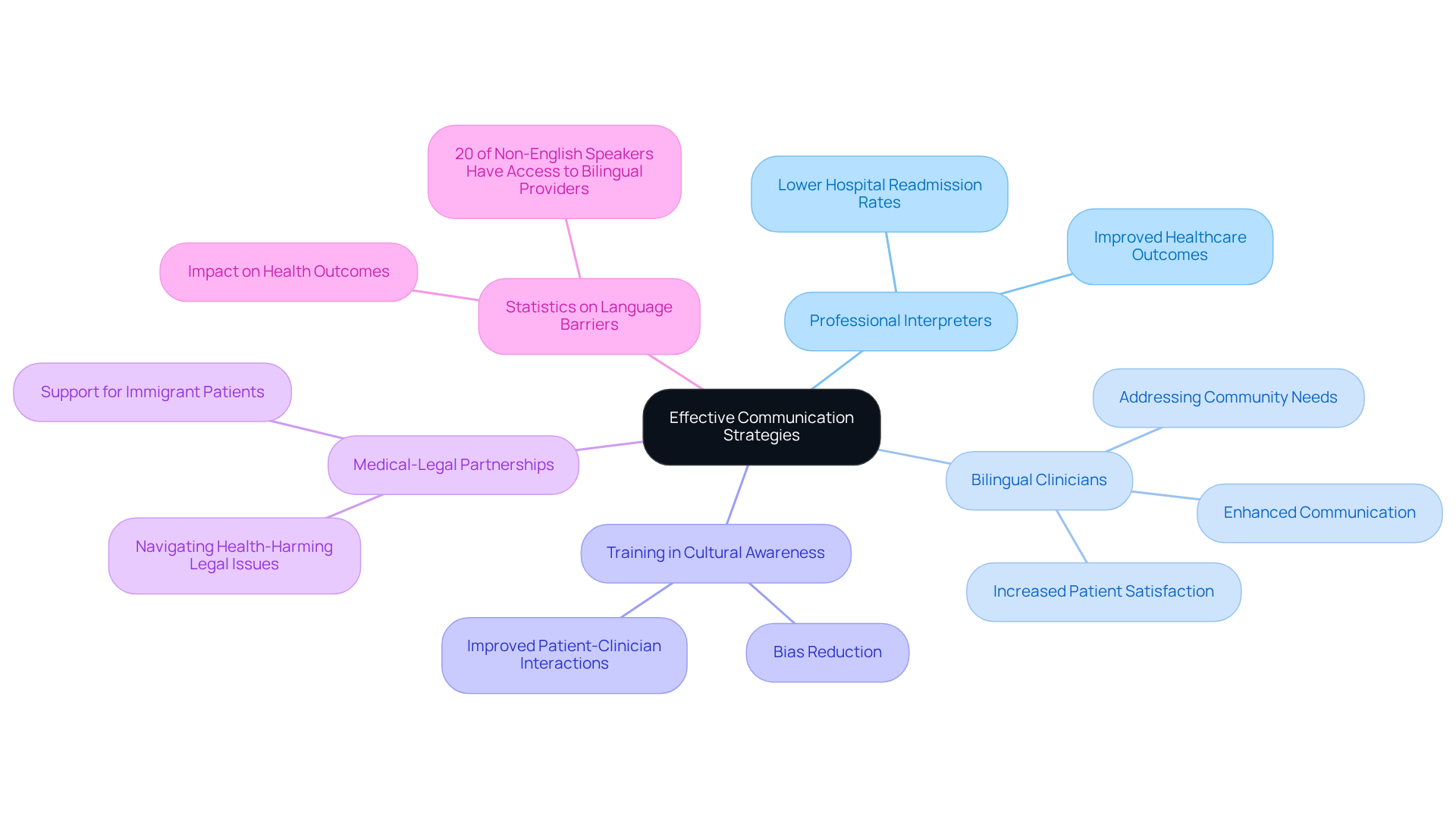
Effective Communication Strategies: Bridging Language Barriers in Healthcare
Effective communication strategies are essential for overcoming language barriers in medical environments. Have you ever felt lost in the healthcare system because of language differences? Employing professional interpreters greatly improves healthcare outcomes. Studies indicate that individuals with limited English proficiency achieve better health results when they can communicate effectively with their medical providers. For instance, individuals receiving home health care who consistently collaborate with the same bilingual nurse report lower hospital readmission rates. This underscores the importance of continuity in care. Yet, there is a pressing need for more in diverse communities to ensure that individuals receive the support they require.
It’s important to know that medical organizations are urged to offer translated resources and ensure employees receive training in cultural awareness and bias education. This training is vital to tackle ethnic and racial prejudices that can adversely affect interactions with clients. By promoting an inclusive atmosphere where foreign-born individuals feel acknowledged and appreciated, healthcare providers can enhance satisfaction and compliance with treatment plans.
Expert viewpoints stress that overcoming language obstacles is not solely about translation; it entails fostering a supportive environment that enables individuals to articulate their needs. Medical-legal partnerships (MLP) can also play a vital role by assisting immigrant individuals in navigating health-harming legal issues, further enhancing their overall care experience. MLP attorneys can help individuals navigate intricate legal circumstances that may influence their health results. Ultimately, a commitment to effective communication can lead to improved health equity and better outcomes for diverse groups of individuals.
It is crucial to highlight that only 20% of individuals who speak a language other than English are visited by a provider who speaks their language. This statistic emphasizes the urgency of addressing these barriers. Moreover, medical staff frequently encounter difficulties when individuals receiving care and their supporters communicate in different languages, which can hinder the provision of services. Remember, you don’t have to face these challenges alone—we’re here to fight for your family.
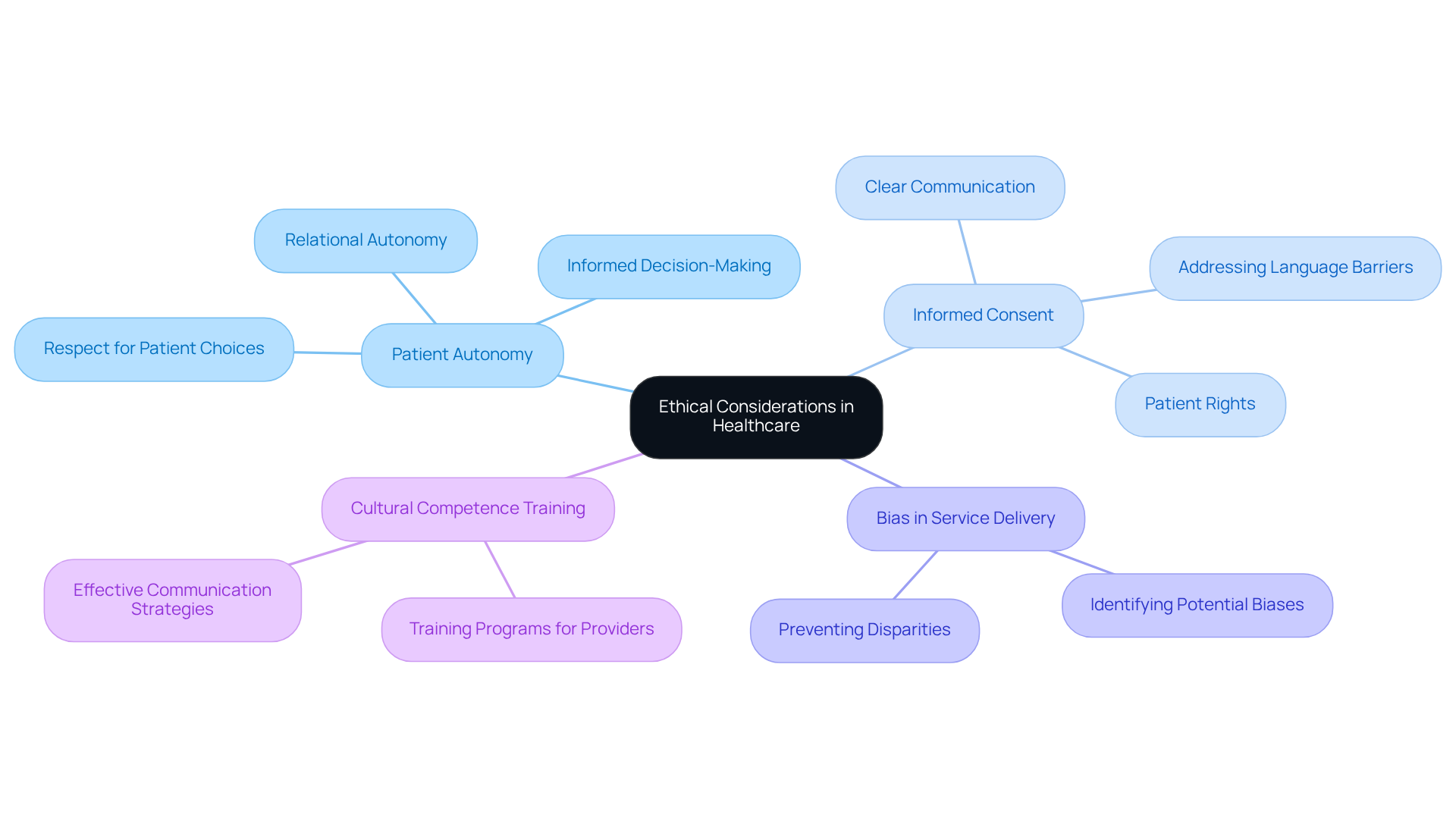
Ethical Considerations in Healthcare: Upholding Standards for Immigrant Patients
Healthcare providers hold a vital responsibility: maintaining ethical standards to ensure fair treatment for immigrant individuals. It’s essential to respect patient autonomy—this builds trust and encourages active involvement in medical decisions. Have you ever felt lost in navigating healthcare? Informed consent must be communicated clearly, especially in diverse populations where language barriers exist. Approximately 8% of Medicare beneficiaries in the U.S. have limited English proficiency, underscoring the need for accessible information.
Moreover, it’s crucial to address potential biases in service delivery to prevent disparities in treatment outcomes. By prioritizing these ethical considerations—beneficence and non-maleficence—healthcare providers can significantly enhance the quality of services for foreign populations. We understand how overwhelming this feels, but there are steps we can take together.
To support these efforts, providers should implement training programs focused on and effective communication strategies. This commitment leads to improved health outcomes and greater client satisfaction. Remember, you’re not alone in this fight; we’re here to support you every step of the way. Your future matters to us, and together, we can make a difference.
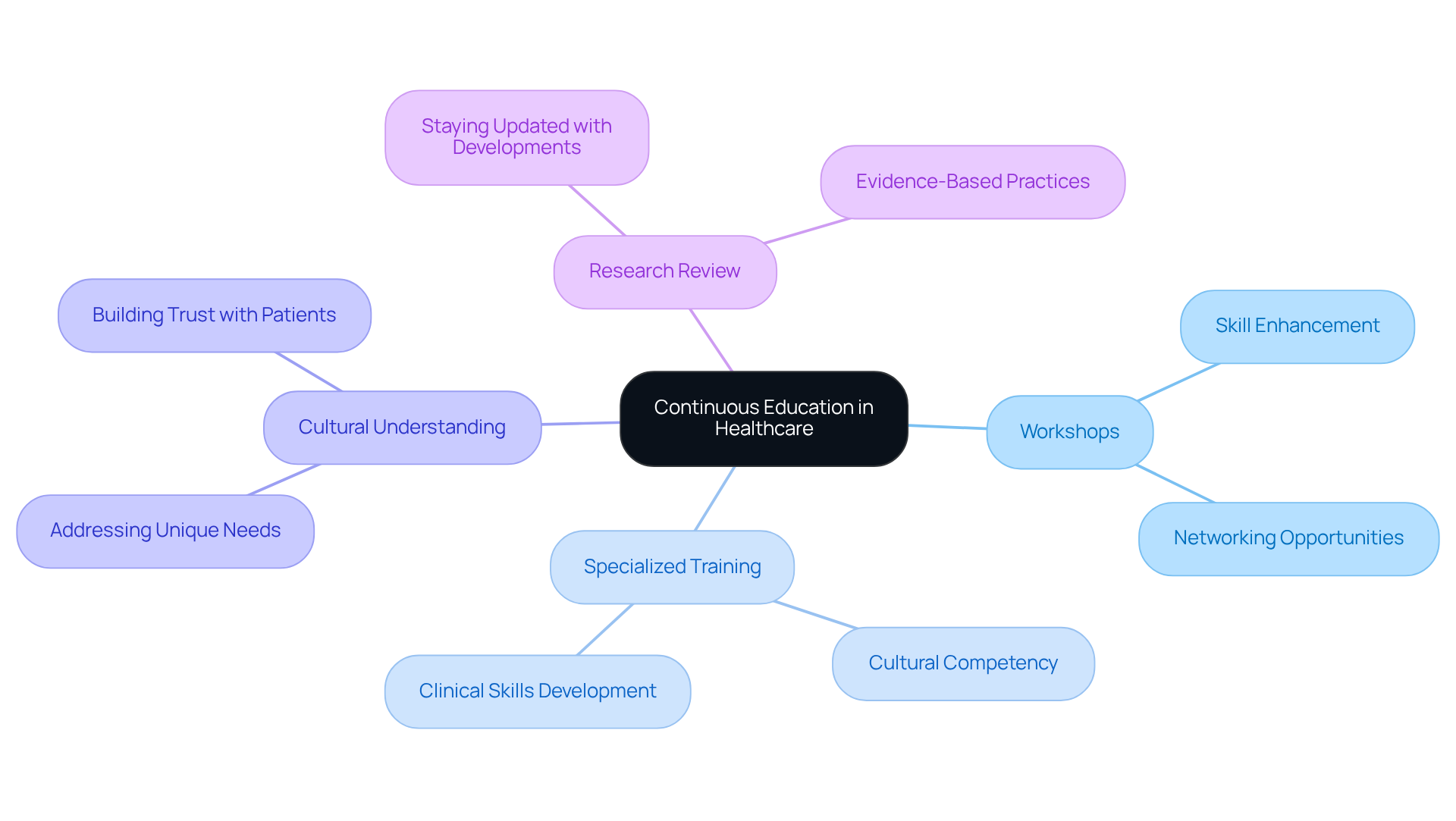
Continuous Education in Healthcare: Staying Informed for Better Patient Care
Healthcare professionals must prioritize ongoing education to stay updated with developments in healthcare, especially concerning the health concerns of newcomers. Have you ever felt overwhelmed by the complexities of accessing care? Engaging in workshops, specialized training programs, and reviewing the latest research are essential steps in this process.
Training initiatives centered on significantly enhance support for diverse population groups, addressing the specific needs and challenges faced by newcomers. Data shows that continuous training improves providers' capacity to offer respectful and culturally aware support. This is vital, considering that 30% of foreign-born adults report difficulties in obtaining such assistance.
We understand how critical this is. Expert views emphasize that lifelong learning not only enhances clinical abilities but also fosters a deeper comprehension of the unique challenges faced by immigrant individuals. By committing to this educational journey, healthcare providers can elevate the quality of care they offer, ensuring that all patients receive the attention and respect they deserve.
Your future matters to us, and we’re here to fight for you.
Conclusion
Garfinkel's ethnomethodology sheds light on the complex dynamics of healthcare interactions, especially for immigrant populations. It emphasizes the importance of social interactions and cultural understanding, laying the groundwork for enhancing the healthcare experiences of newcomers. Recognizing the unique challenges faced by these individuals—such as language barriers and cultural differences—is crucial for creating an inclusive and effective medical environment.
Key arguments throughout this article underscore the necessity of reflexivity among healthcare providers, the demand for tailored communication strategies, and the implementation of culturally competent practices. By engaging in reflexive practices, medical professionals can build trust and improve communication with immigrant patients, ultimately leading to better health outcomes. Additionally, understanding the cultural contexts of diverse populations allows for more personalized care, addressing the specific needs of individuals navigating the healthcare system.
Reflecting on these principles, Garfinkel's ethnomethodology not only strengthens patient-provider relationships but also fosters a more equitable healthcare system. As the healthcare landscape evolves, it is imperative for providers to commit to ongoing education and cultural competence training. This dedication ensures that all individuals, regardless of their background, receive the respectful and comprehensive care they deserve. Embracing these practices is not just beneficial—it is essential for the well-being of immigrant communities and the overall integrity of healthcare systems.
Frequently Asked Questions
What is Garfinkel's ethnomethodology and its relevance in healthcare?
Garfinkel's ethnomethodology examines the everyday practices individuals use to navigate social environments. In healthcare, it helps understand the relationships between patients and practitioners, which significantly influence the quality of care provided.
Why is understanding social interactions important for foreign-born medical professionals?
Understanding social interactions is crucial for foreign-born medical professionals to create an environment where patients feel valued and understood. Positive social interactions lead to increased trust, improved communication, and better health outcomes for these individuals.
What challenges do newcomers face in accessing healthcare?
Many newcomers experience anxiety regarding immigration enforcement, leading them to miss medical appointments and worsening existing health disparities. This anxiety can result in patients canceling or skipping appointments, highlighting the need for supportive social interactions.
How can medical practitioners improve care for foreign populations?
Medical practitioners can enhance care by being attuned to the cultural and linguistic needs of their patients, which improves the quality of care and alleviates the isolation and anxiety newcomers face in clinical settings.
What role does reflexivity play in patient-caregiver relationships?
Reflexivity involves self-examination of personal biases and assumptions during client interactions. This practice is essential for creating an inclusive environment that respects diverse backgrounds, enhances communication, and builds trust with immigrant individuals.
What are breaching experiments and their significance in healthcare?
Breaching experiments reveal how immigrant individuals face cultural differences and systemic barriers in healthcare. They provide insights into the challenges, such as language barriers, that can lead to misunderstandings and dissatisfaction with care.
What statistics highlight the challenges faced by immigrant individuals in healthcare?
Statistics indicate that 25% of immigrant adults struggle with scheduling appointments due to language barriers and cultural misunderstandings, and 29% of Spanish-speaking individuals report unresolved medical conditions after a doctor's visit.
How can medical providers adapt their practices based on breaching experiments?
By conducting breaching experiments, medical providers can uncover hidden expectations and adjust their practices to foster an inclusive atmosphere that respects and supports the diverse cultural backgrounds of newcomers.




